Global Oral Health Perspectives: Addressing Disparities in Dental Care Access and Education
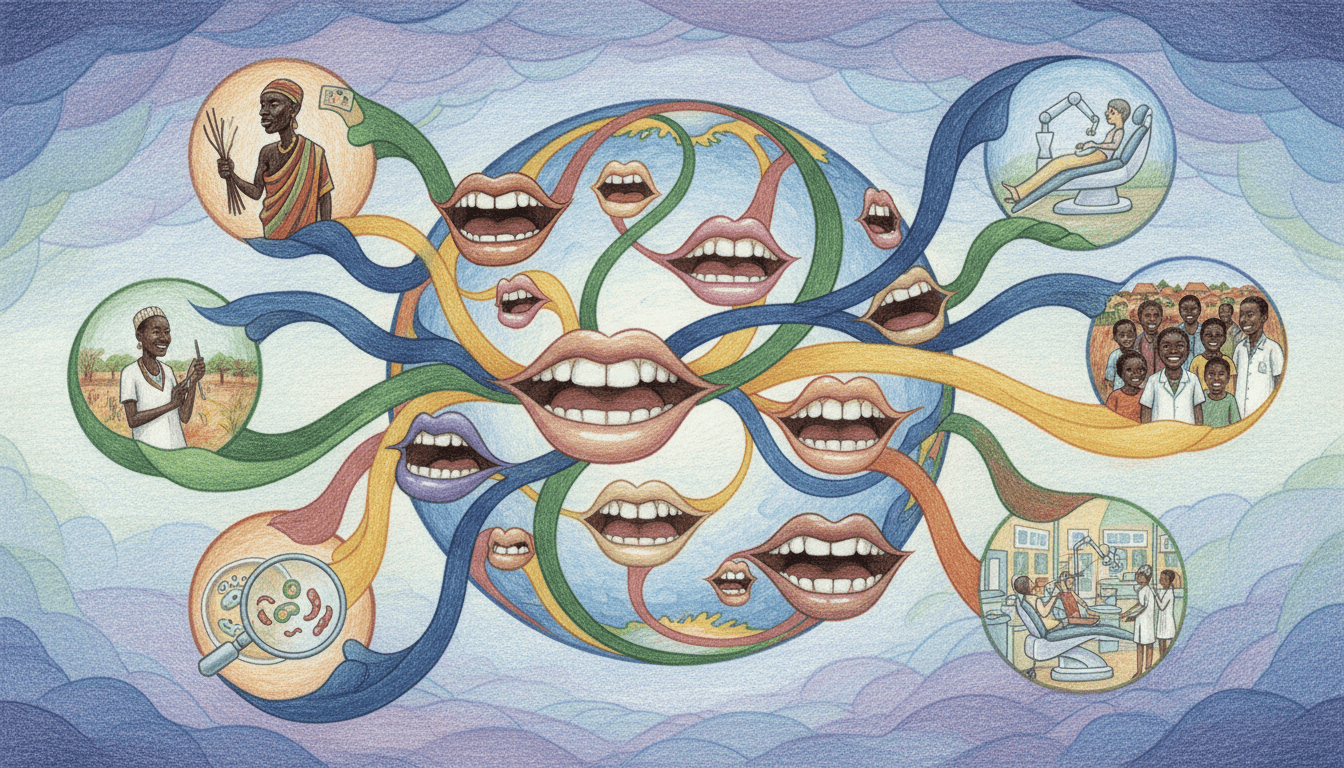
This comprehensive guide explores global oral health perspectives, highlighting significant disparities in dental care access, education, and preventative strategies. Drawing on data from International Dental Health Research, it examines how unequal resource distribution, socioeconomic factors, and varying public health policies impact oral wellness worldwide. The article provides actionable insights for improving dental care accessibility, emphasizes evidence-based preventative approaches, and advocates for integrated educational initiatives to bridge gaps in oral health equity across diverse populations.
Oral health is a critical component of overall well-being, yet global perspectives reveal stark disparities in dental care access, education, and preventative practices. According to International Dental Health Research, approximately 3.5 billion people worldwide suffer from oral diseases, with untreated dental caries affecting nearly half of the global population. These challenges are compounded by unequal access to dental services, varying levels of public health investment, and socioeconomic barriers that disproportionately affect low-income and rural communities. This article delves into the multifaceted nature of global oral health, examining regional variations, systemic inequities, and evidence-based strategies to foster comprehensive dental wellness. By understanding these perspectives, healthcare providers, policymakers, and individuals can collaborate to develop more inclusive and effective oral care frameworks that prioritize equity, education, and prevention.
1Global Variations in Oral Health: Regional Challenges and Trends
2Addressing Dental Care Access Disparities: Strategies for Equity
3Comprehensive Oral Health Education: Empowering Preventative Strategies
4Innovations and Future Directions in Global Oral Health
Key Takeaways
- Global oral health disparities are driven by unequal access to care, education gaps, and socioeconomic factors.
- Preventative strategies, including community fluoridation and school-based programs, can reduce oral disease burden by up to 40%.
- Innovations like teledentistry and AI diagnostics are pivotal for expanding care in underserved regions.
- Policy reforms and international collaborations are essential to achieve oral health equity worldwide.
Frequently Asked Questions
What are the main barriers to dental care access in low-income countries?
Key barriers include financial constraints (e.g., high out-of-pocket costs), shortages of dental professionals (dentist-to-population ratios as low as 1:150,000), and geographic isolation. Limited public health infrastructure and lack of insurance coverage further exacerbate these challenges, leading to higher rates of untreated oral diseases.
How can individuals contribute to improving global oral health?
Individuals can advocate for policy changes, support NGOs providing dental care in underserved areas, and practice preventative habits like brushing with fluoride toothpaste and reducing sugar intake. Sharing evidence-based information within communities also helps raise awareness and combat misinformation about oral hygiene.
Why is oral health education critical for preventative care?
Education empowers people to adopt healthy behaviors early, reducing the risk of cavities, gum disease, and other conditions. Studies show that comprehensive school-based programs can decrease childhood caries by 40%, while adult education on oral-systemic links encourages timely dental visits and better overall health outcomes.
What role does technology play in addressing oral health disparities?
Technology, such as teledentistry and AI diagnostics, enables remote consultations and early detection of issues, making care more accessible in rural or resource-poor areas. Mobile apps and digital platforms also facilitate education, helping bridge knowledge gaps and promote consistent oral hygiene practices globally.
Conclusion
Global oral health perspectives reveal both challenges and opportunities for creating a more equitable dental care landscape. By addressing disparities in access, enhancing education, and leveraging innovations, stakeholders can make significant strides toward reducing the burden of oral diseases. As International Dental Health Research underscores, collaborative efforts—spanning governments, healthcare providers, and communities—are vital for fostering preventative strategies and ensuring that oral wellness becomes a universal reality. Through sustained commitment and evidence-based actions, we can build a future where everyone, regardless of location or socioeconomic status, enjoys the benefits of a healthy smile.