Oral Hygiene and Overall Health Connection: The Critical Link Between Dental Care and Systemic Wellness
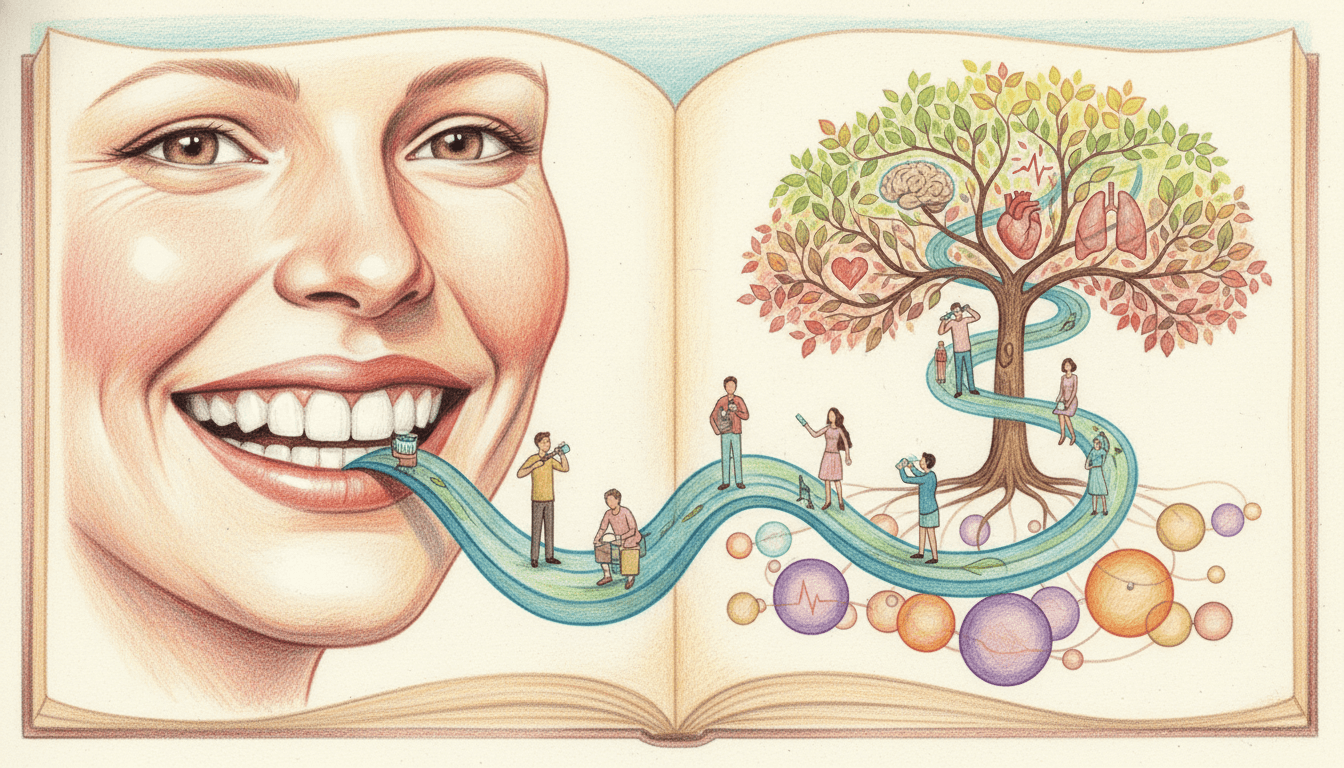
This comprehensive guide explores the profound connection between oral hygiene and overall health, detailing how poor dental care can contribute to serious conditions like heart disease, diabetes, and stroke. Backed by medical research, it emphasizes that oral health is not isolated but integral to systemic wellness. The article provides evidence-based insights into the mechanisms linking gum disease to broader health issues and outlines essential daily practices—brushing, flossing, and mouthwash use—to mitigate risks. Aimed at promoting a holistic approach, it underscores the importance of consistent oral hygiene for long-term health benefits.
Oral hygiene is far more than just maintaining a bright smile; it is a critical component of overall health. Research from medical and dental studies consistently shows that the state of your mouth can significantly influence systemic conditions, including cardiovascular diseases, metabolic disorders like diabetes, and immune function. Poor oral health, particularly gum disease (periodontitis), allows harmful bacteria to enter the bloodstream, triggering inflammation and contributing to chronic illnesses. This article delves into the science behind these connections, highlighting key risks such as heart disease, stroke, and diabetes, while providing actionable strategies for effective oral care. By understanding and implementing a thorough hygiene routine, individuals can protect not only their teeth and gums but also their long-term wellness.
1The Science Behind Oral-Systemic Health Connections
2Key Health Risks of Poor Oral Hygiene
3Essential Daily Oral Hygiene Practices
4The Role of Professional Dental Care in Systemic Health
Key Takeaways
- Oral health is intrinsically linked to systemic conditions like heart disease, diabetes, and stroke.
- Gum disease allows bacteria to enter the bloodstream, causing inflammation that harms organs.
- Daily brushing, flossing, and mouthwash use are essential to reduce health risks.
- Professional dental care enhances systemic wellness, especially for chronic disease management.
- A holistic approach to oral hygiene supports long-term immune and cardiovascular health.
Frequently Asked Questions
How exactly does poor oral hygiene lead to heart disease?
Poor oral hygiene, particularly gum disease, allows bacteria to enter the bloodstream, where they can attach to fatty plaques in arteries. This triggers inflammation, leading to atherosclerosis (narrowing of arteries), which increases the risk of heart attacks and strokes. Studies show that treating gum disease can reduce systemic inflammation markers like C-reactive protein, lowering cardiovascular risk.
Can improving oral health help manage diabetes?
Yes, effectively managing oral health, especially through treatment of gum disease, can improve blood sugar control in diabetics. Research indicates that periodontal therapy can lead to modest reductions in HbA1c levels (by 0.4-0.6%), making diabetes easier to manage and reducing complications like nerve damage and kidney issues.
What is the most overlooked part of a daily oral care routine?
Flossing is often neglected but is critical because it removes plaque and bacteria from between teeth and under the gumline, areas that brushing alone cannot reach. Skipping flossing leaves up to 40% of tooth surfaces unclean, increasing the risk of gum disease and its systemic health consequences.
How often should I visit the dentist to support overall health?
It is generally recommended to visit the dentist every six months for check-ups and cleanings. However, individuals with existing health conditions like heart disease or diabetes may benefit from more frequent visits (e.g., every 3-4 months) to monitor and manage oral health risks effectively.
Conclusion
The connection between oral hygiene and overall health is undeniable and supported by extensive medical research. By maintaining a consistent routine of brushing, flossing, and using mouthwash, along with regular dental visits, individuals can significantly reduce their risk of serious conditions like heart disease, diabetes, and stroke. Oral care should be viewed as an integral part of a holistic health strategy, not an isolated practice. Embracing this approach empowers people to protect their systemic wellness while achieving a healthier smile. As studies continue to reveal new insights, the importance of oral health in preventive medicine will only grow, making it essential for everyone to prioritize their dental care.